The Road to Treatment: Insurance Woes
I can’t remember the first time I heard the phrase “cut through the red tape,” but those words didn’t really affect me until I tried to get an approval for MS treatment.
At this time, there are 13 treatments for MS…
-Injectables: Avonex, Betaseron, Copaxone, Extavia, Glatopa, Plegridy and Rebif.
-Oral medications: Aubagio, Gilenya and Tecfidera.
-Infusions: Lemtrada, Novantrone and Tysabri.
I was given two options … more on that in my next post. Once I chose my treatment, the next step was picking a place to receive it. Once that was decided, the hospital where I was diagnosed (University of Chicago) connected with Blue Cross to confirm coverage. Then, the drug company did the same. (But they also gave me the unpleasant news that insurance company doesn’t always cover treatment, because it’s so expensive … about $5,000+ per treatment). Then, it was the treatment center’s turn.
I waited about a week and didn’t hear anything. I called the drug company and left message. A few days later, on a Friday, I received a call and was told I would be 100 percent covered once I hit my out-of-pocket maximum and to go ahead and make an appointment for my first treatment. Good news, I thought.
Since it was the weekend, I waited until Monday to call the treatment center. When I called, I was asked if I had received a call from them to make an appointment. When I said that the drug company told me the insurance approval came through and the drug company told me to call, I was then told that the approval didn’t come through yet. “We resubmitted the paperwork on Friday and are awaiting the approval.”
 Confused, I hung up and became distraught. I connected with the insurance company to find out what was taking them so long. Turns out, the treatment center goofed up on the paperwork. The submission for approval contained a code for one medication (one I didn’t choose) and the description of another (the one I chose). When Blue Cross tried to reach the center by phone, no one answered. So then, the policy is to send a letter to both the center and the patient.
Confused, I hung up and became distraught. I connected with the insurance company to find out what was taking them so long. Turns out, the treatment center goofed up on the paperwork. The submission for approval contained a code for one medication (one I didn’t choose) and the description of another (the one I chose). When Blue Cross tried to reach the center by phone, no one answered. So then, the policy is to send a letter to both the center and the patient.
After I hung up with Blue Cross, I then got the day’s mail and, low and behold, there was a letter from Blue Cross. It contained the same information I learned on the phone. So when the treatment center told me they “resubmitted the paperwork,” it was because they made a mistake. They conveniently left that part out when I called.
Because of a mistake, the approval process took an extra 15 business days. The process, which should have taken 7 to 14 days, took over a month. And, for some reason, someone from the drug company mistakenly told me I was covered … instead of telling me what the coverage would be IF I WAS APPROVED.
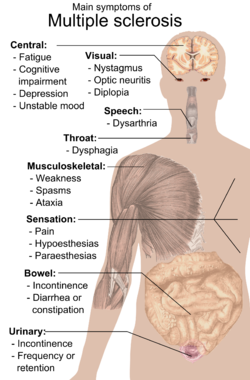
I know mistakes happen, I’m just upset that I had to pay for it. And while I know the treatment won’t “fix” my symptoms, I know it does stop the progression of the disease. So, I have to think that gives my body (and brain) a good chance to enter a remission period. That said, my treatment finally starts this Sunday. So, I’ll be back with more on my decision, the information about the medication and my experience with the first treatment.
Photo courtesy Wikipedia
welcome to today’s world of healthcare. However, keep up with your positive attitude. That’s one thing you have total control over.